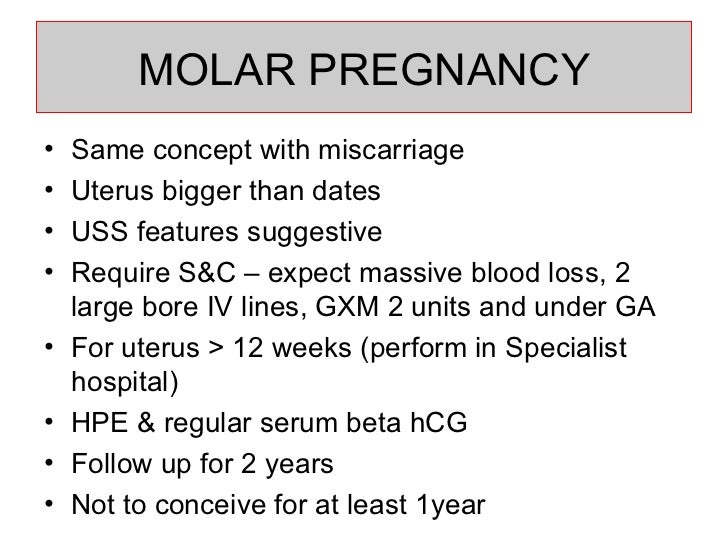
Hydatidiform Mole (Molar Pregnancy)
11:54:00 AM



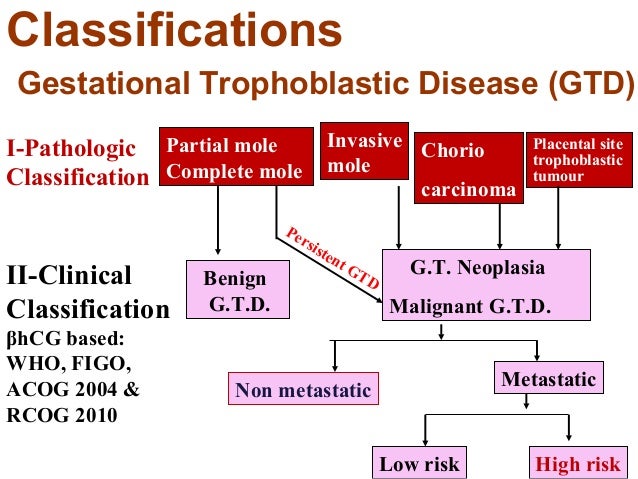


Hydatidiform Mole Clinical Presentation
Updated: Nov 15, 2016
Author: MEDSCAPE
History
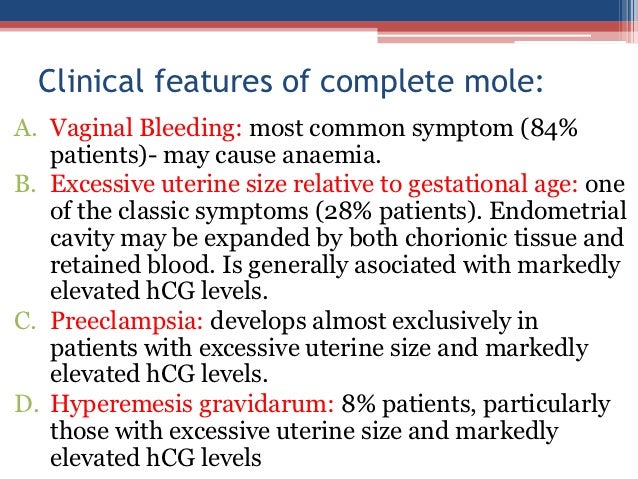
Complete mole
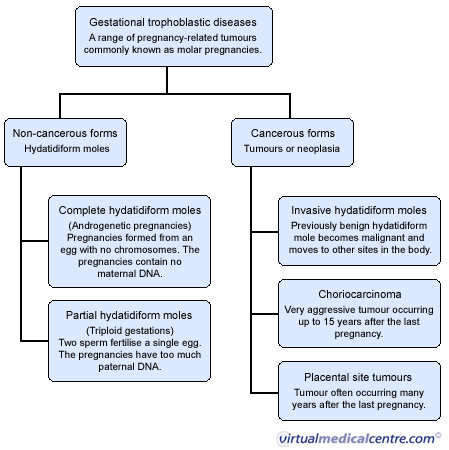
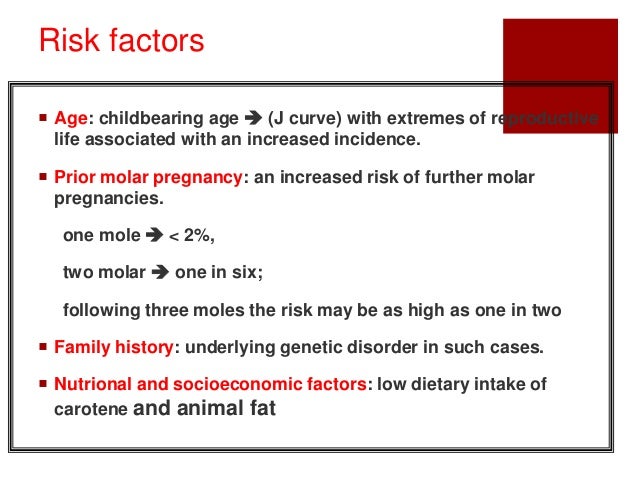
The typical clinical presentation of complete molar pregnancies has changed with the advent of high-resolution ultrasonography. Most moles are now diagnosed in the first trimester before the onset of the classic signs and symptoms.
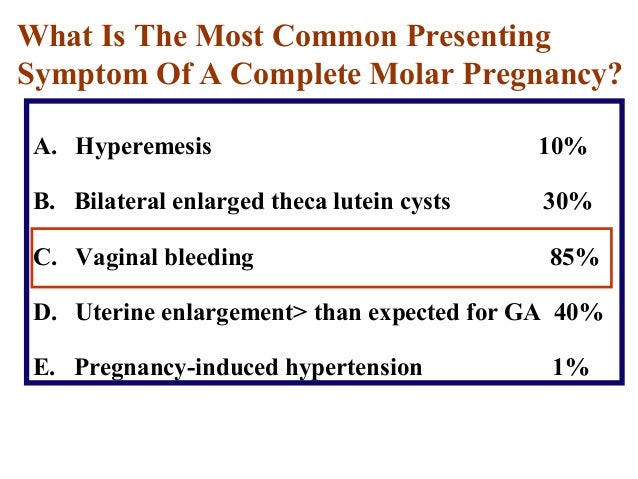
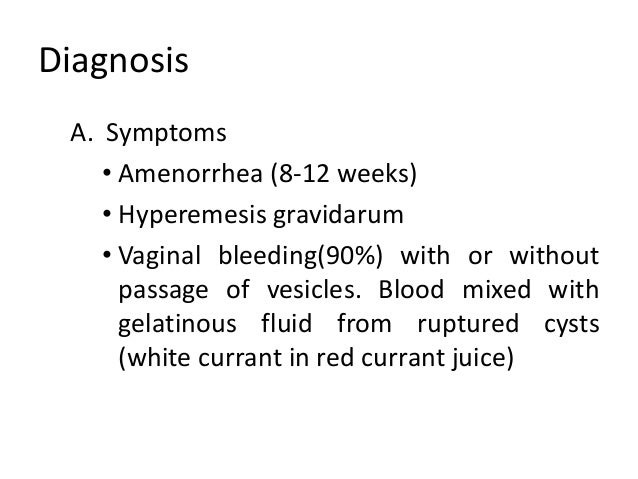
Vaginal bleeding
The most common classic symptom of a complete mole is vaginal bleeding. Molar tissue separates from the decidua, causing bleeding. The uterus may become distended by large amounts of blood, and dark fluid may leak into the vagina. This symptom occurs in 50% of cases.
Hyperemesis
Patients may also report severe nausea and vomiting. This is due to extremely high levels of human chorionic gonadotropin (hCG). This is reported to occur in 4% of patients diagnosed at 5-9 weeks of gestation, and in 23% when the diagnosis is made after 10 weeks' gestation.
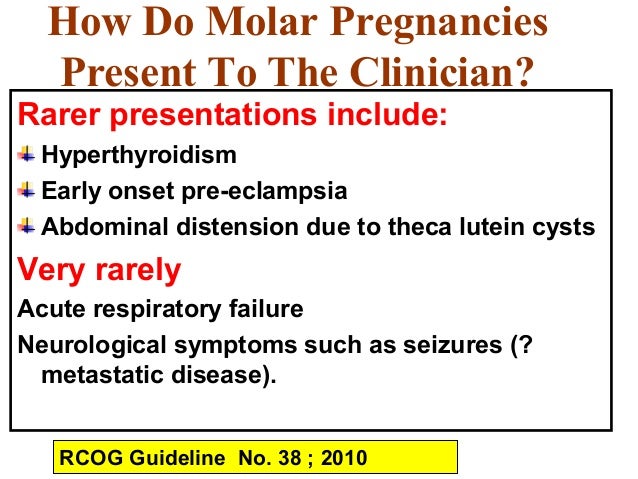
Hyperthyroidism
Signs and symptoms of hyperthyroidism can be present due to stimulation of the thyroid gland by the high levels of circulating hCG or by a thyroid stimulating substance (ie, thyrotropin) produced by the trophoblasts. Clinical hyperthyroidism has been reported in 3.7% of women with a hydatidiform mole diagnosed after the 10th week of gestation.
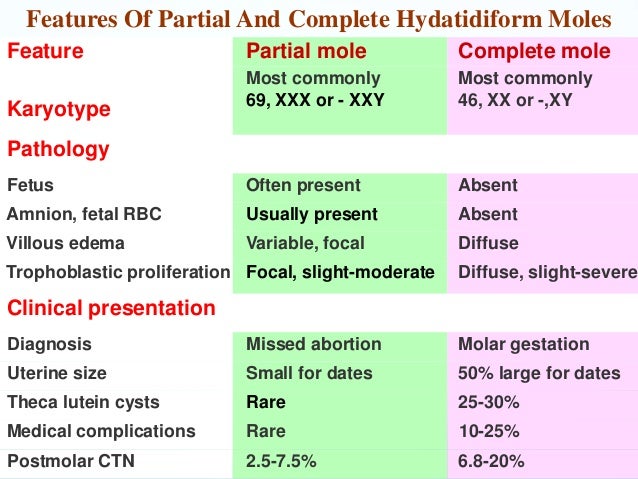
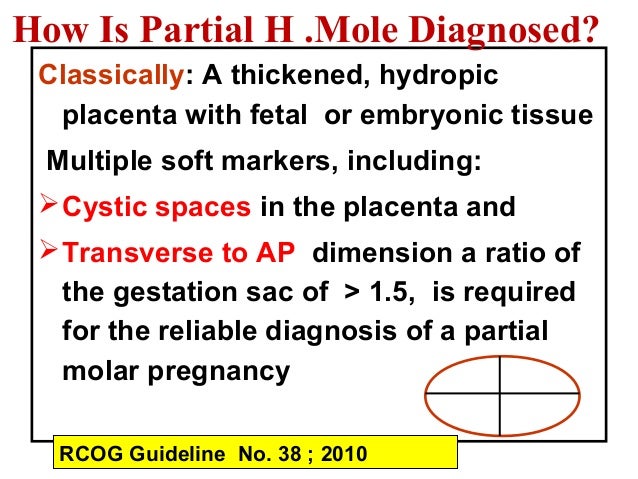
Partial mole
Patients with partial mole do not have the same clinical features as those with complete mole. These patients usually present with signs and symptoms consistent with an incomplete or missed abortion, including vaginal bleeding and absence of fetal heart tones.
In a retrospective study (1994-2013) at a Brazilian trophoblastic disease center, investigators evaluated the clinical presentations and incidence of postmolar gestatoinal trophoblastic neoplasia (GTN) among 355 women with complete mole (n =186) or partial mole (n = 169), with the following findings [32] :
- Risk of vaginal bleeding, biochemical hyperthyroidism, anemia, uterine size larger than dates, and hyperemesis: Reduced risk in women with partial mole
- Preevacuation serum hCG levels: Lower in women with partial mole
- Median gestational age at evacuation: complete mole, 9 weeks; partial mole, 12 weeks
- Development of GTN: women with complete mole, 17.7%; women with partial mole, 4.1%
Those with complete mole were diagnosed more commonly before evacuation than women with partial mole because they presented more often with signs/symptoms of molar disease.
Physical Examination
Complete mole
Note the following:
- Size inconsistent with gestational age: A uterine enlargement greater than expected for gestational age is a classic sign of a complete mole. Unexpected enlargement is caused by excessive trophoblastic growth and retained blood. However, patients also present with size appropriate or smaller than expected for the gestational age.
- Preeclampsia: Pelvic ultrasonography has resulted in the early diagnosis of most cases of hydatidiform mole and preeclampsia is seen in less than 2% of cases.
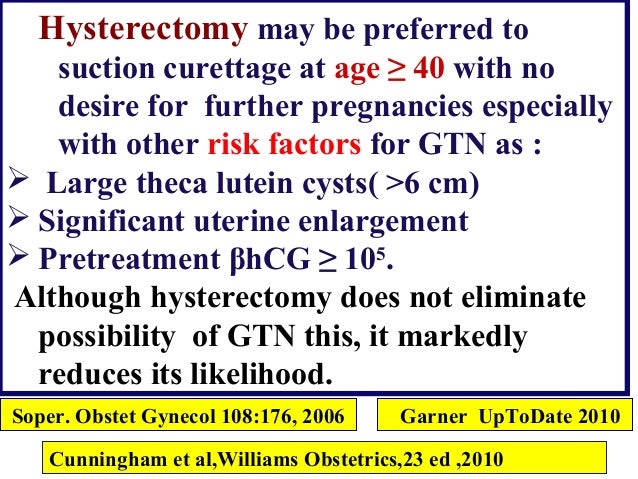
- Theca lutein cysts: These are ovarian cysts greater than 6 cm in diameter and accompanying ovarian enlargement. These cysts are not usually palpated on bimanual examination but are identified by ultrasonography. Patients may report pressure or pelvic pain. Because of the increased ovarian size, torsion is a risk. These cysts develop in response to high levels of beta-hCG. They are reported in 11% of cases diagnosed at longer than10-weeks' gestational age. The cysts spontaneously regress after the mole is evacuated, but it may take up to 12 weeks for complete regression.
Partial mole
Uterine enlargement and preeclampsia is reported in only 5% of patients. Theca lutein cysts, hyperemesis, and hyperthyroidism are extremely rare.
Twinning
Twinning with a complete mole and a fetus with a normal placenta has been reported (see image below). Cases of healthy infants in these circumstances have been reported.
Women with coexistent molar and normal gestations are at higher risk for developing persistent disease and metastasis. Termination of pregnancy is a recommended option.
The pregnancy may be continued as long as the maternal status is stable, without hemorrhage, thyrotoxicosis, or severe hypertension. The patient should be informed of the risk of severe maternal morbidity from these complications.
Prenatal genetic diagnosis by chorionic villus sampling or amniocentesis is recommended to evaluate the karyotype of the fetus.




Laboratory investigations
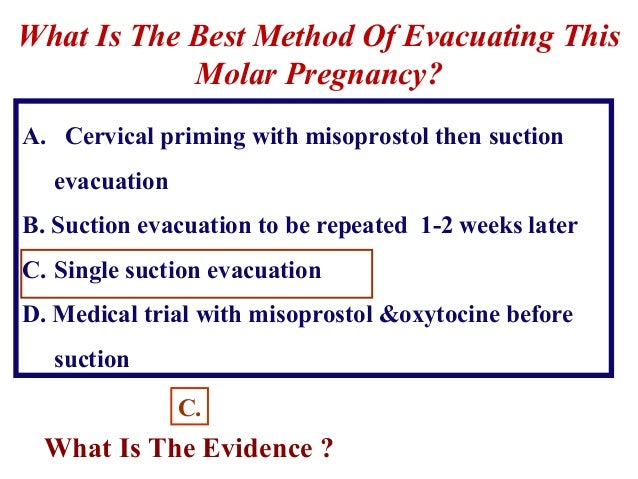
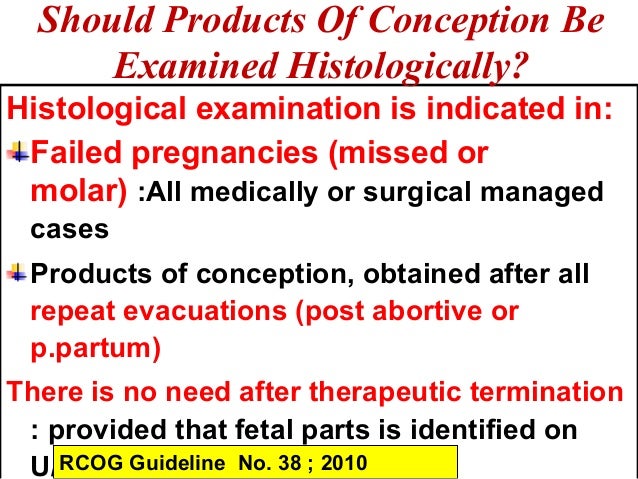
Most molar pregnancies are diagnosed incidentally at pathological evaluation of an evacuated dilation and evacuation (D&E) specimen for missed abortion, or from early maternal ultrasound screening in the first trimester of pregnancy. Remarkably, many women who are diagnosed with molar pregnancy at an early maternal ultrasound screening in the first trimester of pregnancy terminate pregnancy before the development of the classic signs and symptoms. For this reason most authorities consider it mandatory to conduct histological examination of miscarriage tissue.
In all patients with suspected molar pregnancy, the following laboratory investigations are indicated:
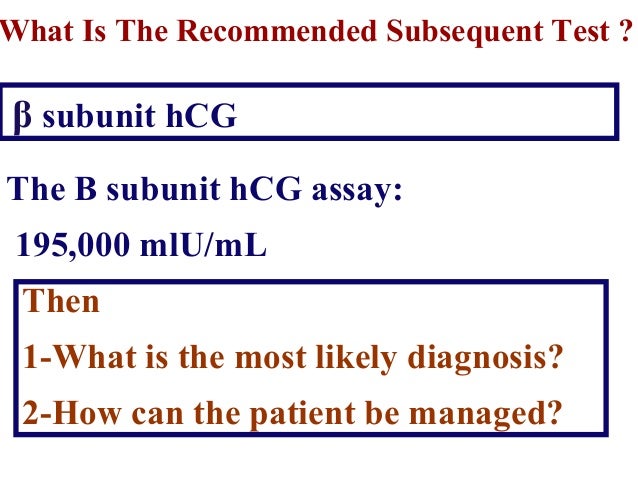
- Serum beta hCG
- FBC
- Serum PT and PTT
- Serum urea, creatinine, LFTs
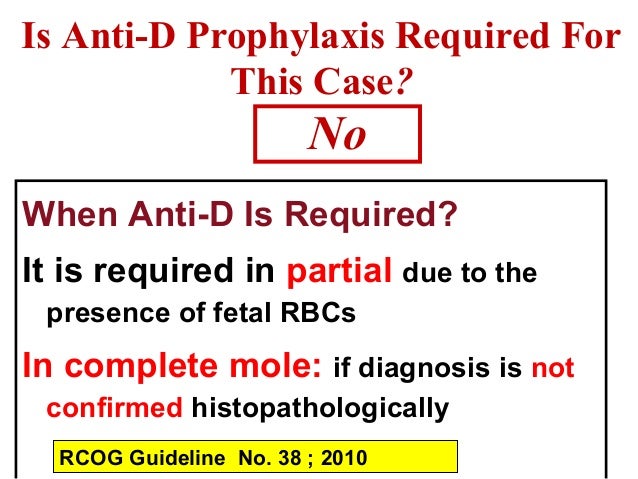
- Blood type with antibody screen
- Thyroid function tests.
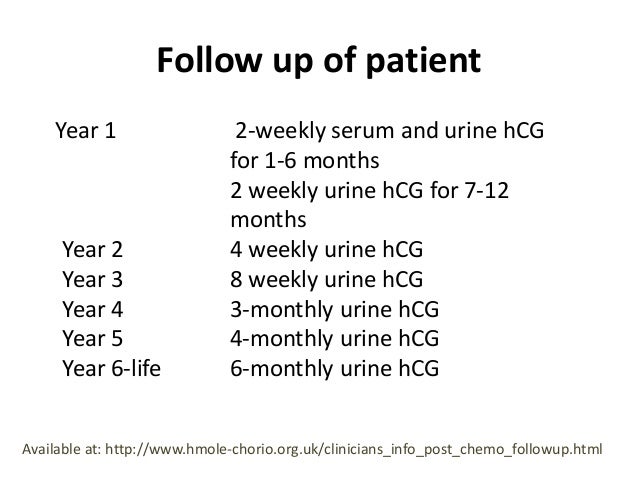
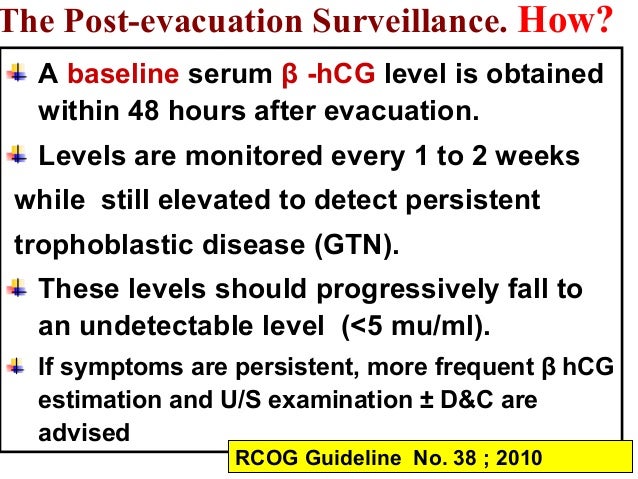
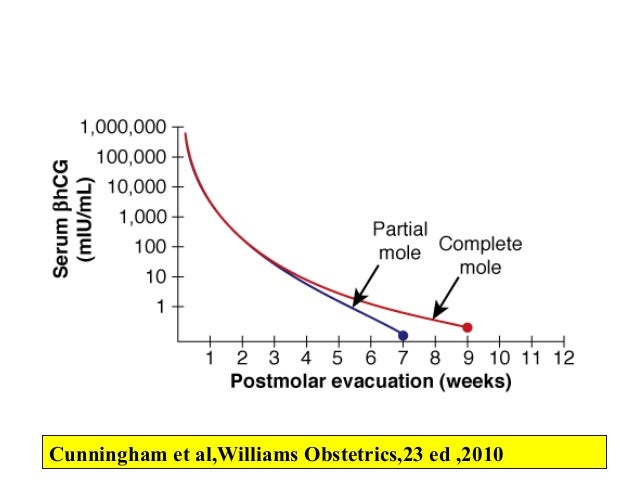
Beta hCG is secreted by syncytiotrophoblasts, which proliferate excessively in molar pregnancy. Normal pregnancies are associated with a peak serum beta hCG of <100,000 IU/L (100,000 mIU/mL). Serum beta hCG acts as a tumour marker to follow post-molar regression, and to identify post-molar gestational trophoblastic neoplasia.
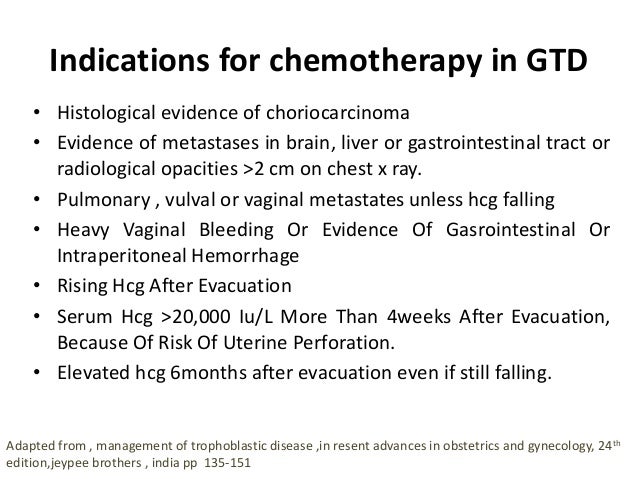
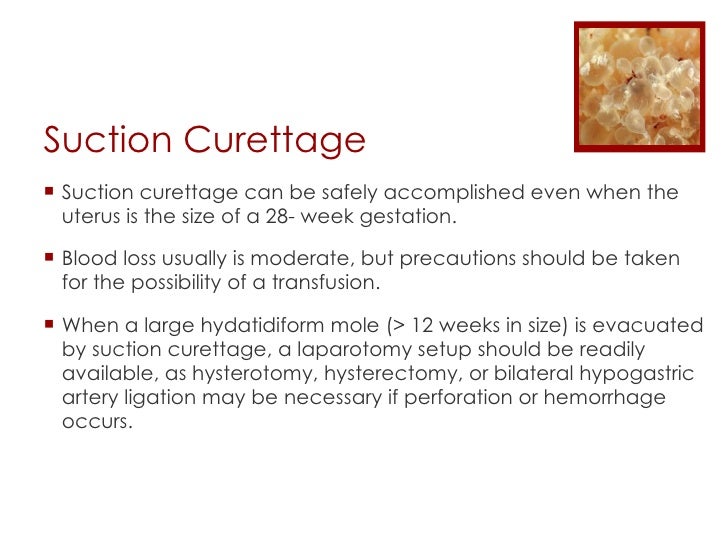
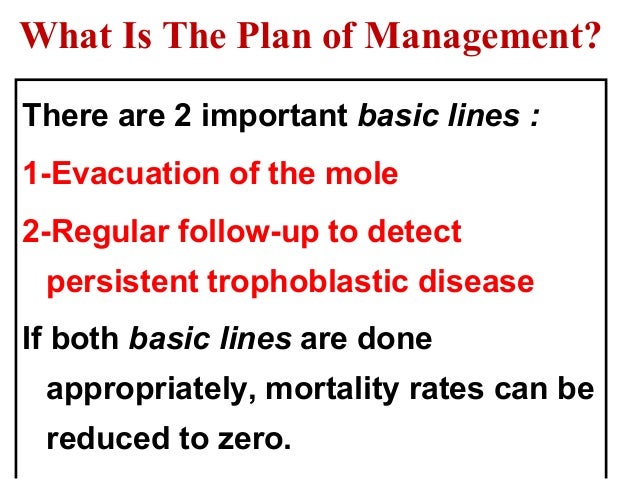
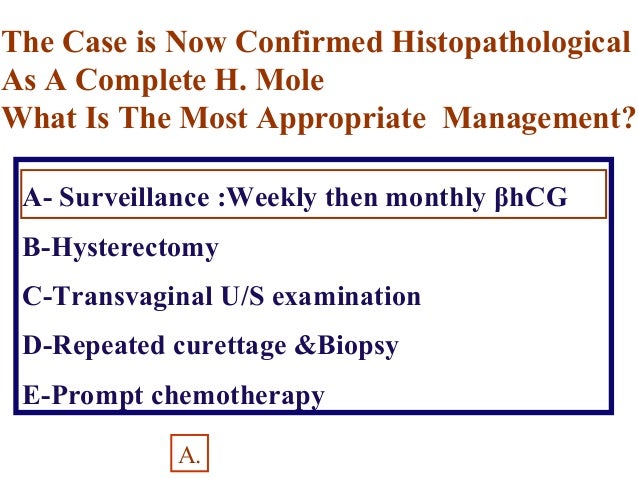
Severe anaemia may result from persistent vaginal bleeding and the dilutional effects of increased blood volume. There is a greater risk for serious bleeding at the time of evacuation for GTD, with a risk of DIC from blood loss or trophoblastic embolism. It is important to establish baseline normal coagulation function and to correct abnormalities before evacuation. About 20% of patients with complete molar pregnancies and 5% of patients with partial molar pregnancies will develop malignant sequelae and require chemotherapy. These chemotherapy agents require normal liver and renal function for optimal dosing. A patient undergoing evacuation of a molar pregnancy is at increased risk for developing bleeding significant enough to require a blood transfusion. Blood typing insures that type-appropriate blood can be made available in the event of haemorrhage.
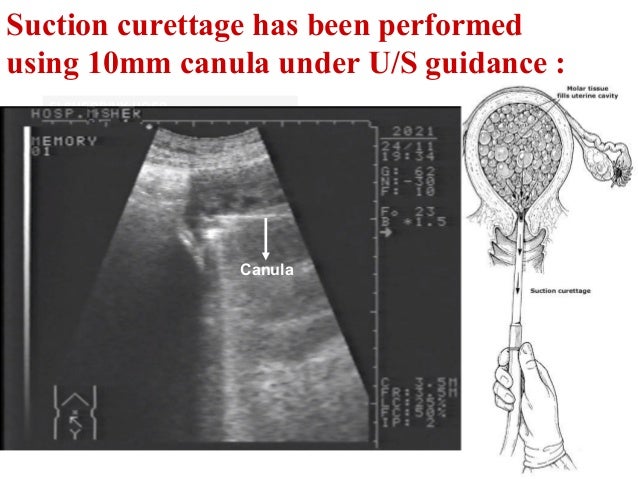
Imaging
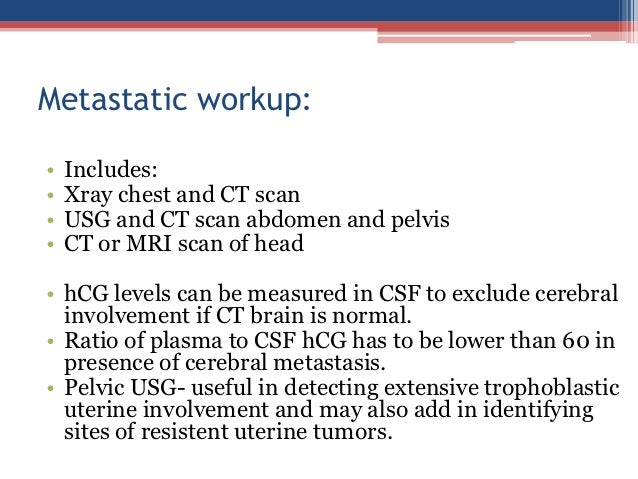
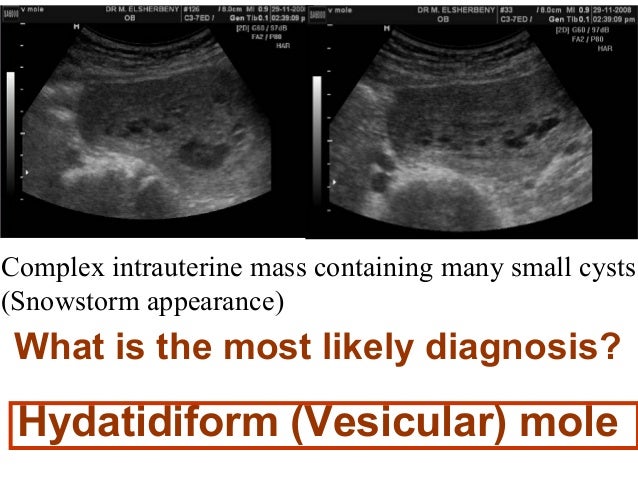
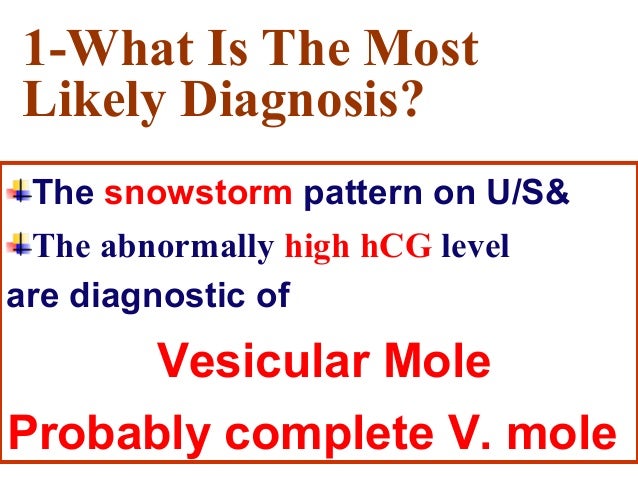
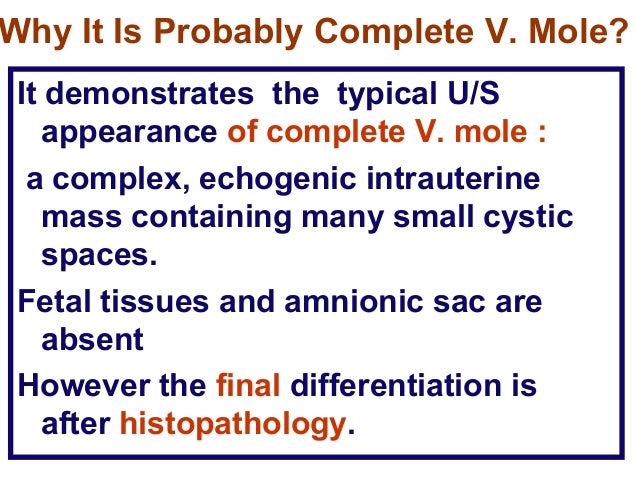
Pelvic ultrasound is the mainstay of diagnosis. Typical ultrasound findings for a complete molar pregnancy include a diffuse echogenic pattern described as a snow-storm pattern, which is created by intermingling of hydropic villi and blood clots. The presence of a smaller volume of abnormal placenta with partial fetal development, without fetal cardiac activity, is characteristic of a partial molar pregnancy. Cystic enlargement of the ovaries may represent theca lutein cysts.
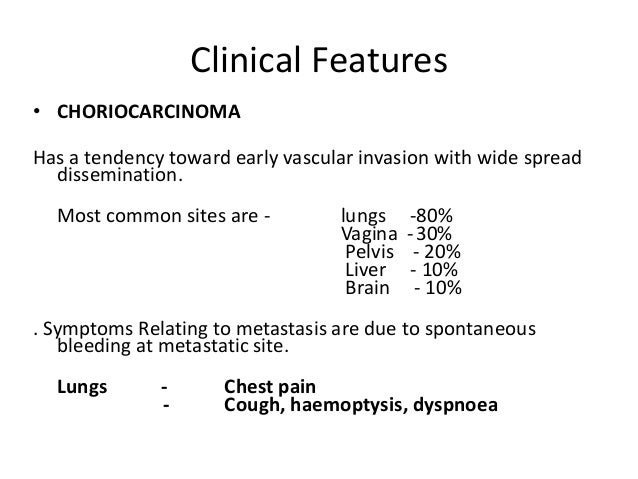
A CXR should be part of any evaluation for suspected or confirmed hydatidiform mole. Pulmonary congestion, oedema, alveolar infiltrates, and metastatic nodules may be visible.

ULTRASOUND
A. Partial MoleB. Complete Mole - Snowstorm Appearance

Molar Pregnancy Algorithm


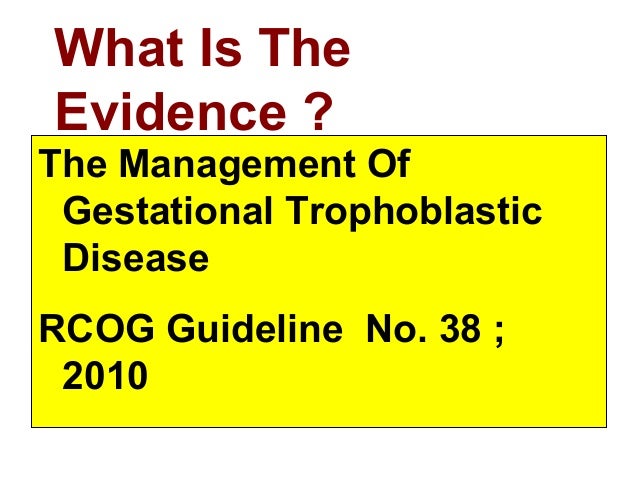
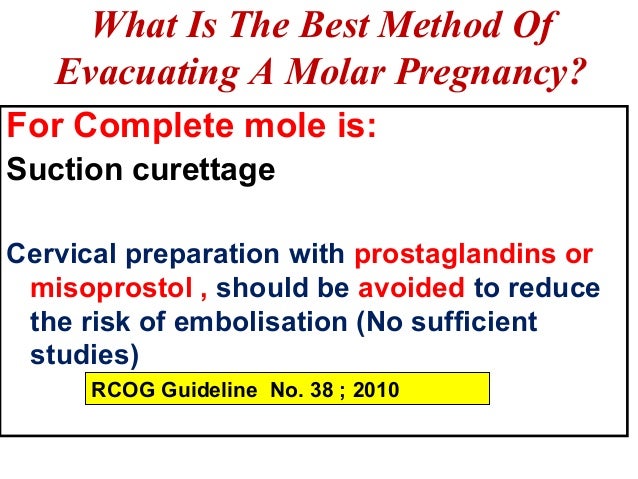
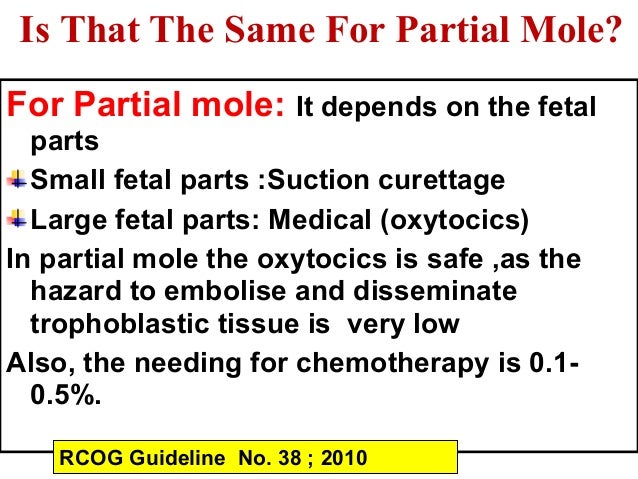
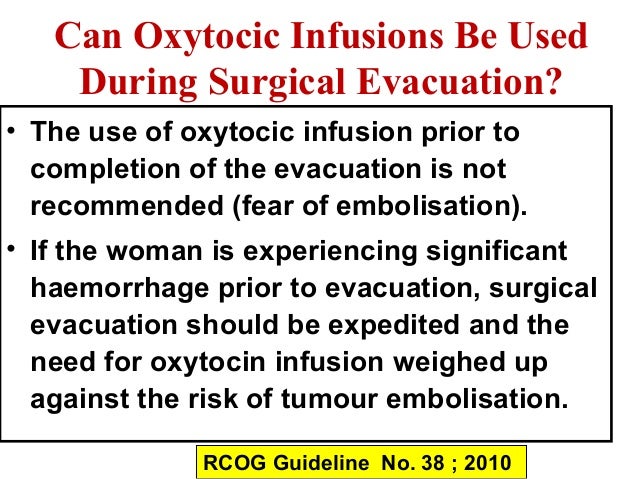
Reference
- Medscape
- RCOG
- NICE Guidelines
- ACOG
- Obstetrics by Ten Teachers 19th Edition
- BMJ Practice
- Slideshare

















0 comments