SURGERY POSTING : LONG CASE END POSTING EXAM
1:39:00 PM
Omgg today is the day for my long case examination. In the long case, the student is required to clerk the patient's history and perform related physical examination on the patient. Then, present the case to the examiners in charged.
My day started early with Bobo's miaww-ing very loud. It's 4.30 am and I'm so sleepy. I slept at 3 am and I need to be at the hospital by 7.15 am. I was told by my leader to gather at Ward Anggerik that morning. Ward Anggerik is for the pediatric patient. I got to know that I need to be there at 7.30 am and gather in a pediatric ward, one of my examiners must be Mr. T. I was so nervous because pediatric surgery is like a whole new chapter for me and I was prepared for adult cases. So I stayed up late till 3 am to cover all the common diseases in paediatrics.
I walked into the ward and noticed something not right. No one there. Mdm Ita also not there yet. I called my friend and she said she was on her way. I called Mdm Ita and she asked me to wait at the sofa area. Sofa area? Where the heck is sofa area? Ah, it took me almost 10 min to realise that I'm at the wrong ward. Confident sungguh pusing kanan tadi. I'm actually in Ward Puteri, which is for internal medicine female ward. Sighhh. Ward Anggerik is at the opposite side of Ward Puteri.
I went to Ward Anggerik and saw Aina was there, reading her notes thoroughly. She smiled at me and said she was nervous. Our senior said yesterday they got pediatric cases like appendicitis, Hirschsprung disease and inguinal hernia. I take out my notes and started to read. Then Gay, Nashriq and Izzati arrived. They also seem nervous. Dr. Saleha came to us and told Aina about her patient. Her patient is in ward 29, bed 3. We were surprised because all of us prepared for pediatric cases hahaha. Mine also in ward 29, bed 5. Aina smiled, speechless to me. I know that feeling. Dah la tak prepare apa apa for Urinary tract diseases!
Okay. Calm down. I went upstairs and saw my patient lying on the bed. A young man, looks comfortable and not in pain? Why is he here..... Ward 29 is for all those urinary tract diseases and disorders. So, I don't expect this patient is having any of those complicated diagnoses. Hmm, my mind running wild at that time. Aina was clerking her patient. Her patient is an old gentleman, probably at his 60. I went to my patient and confirmed that he is my patient.
Patient's file was on that cardiac table and I really want to take a peek on those documents... but I know this is an examination, I dare not to. I flip close the file and arrange it neatly beside me. He was admitted yesterday. I asked why is he here for?
The patient told me he has abdominal pain, initially was at epigastric area then radiated to right iliac fossa. I smiled. Man, this is appendicitis! Hoooorayyyy. So all went smooth. I minta tolong mak cik depan teman I jadi chaperon waktu I examined the patient. Gila kau nak examine berdua - duaan aku dengan dia, dah la nak suruh dia exposed badan dia. Awkward but I dah biasa. It's a routine in the hospital.



So here is the summary of my cases:
The patient is a 24-year-old Malay gentleman, came with a complaint of abdominal pain 1 day prior to admission. This is day 2 of admission. The pain was described as stabbing in nature with sudden onset and continuous. Initially, it was at epigastric area then radiated to right iliac fossa, not associated with fever and vomiting. The pain was aggravated by lying flat and relieved by sitting position. Pain score given was 8/10. Smoke 4 pack-years and no known medical illness (NKMI)
On examination,
The patient was conscious, alert and comfortable lying flat with a cannula attached on his left dorsal hand, connected to Dextrose 5%.
Hand and nails examination were normal. Pulse was 68 bpm with good volume and regular rhythm. Blood pressure was 110/70 mmHg, Temperature was 37-degree celsius and Respiratory rate was 20.
Moving on to face examination, sclera was white and conjunctiva was pink (not pallor). Patient has good oral hygiene, the tongue was moist and no central cyanosis. Throat was not injected. No lymphadenopathy. No lower limb oedema.
Lung was clear, equal air entry bilaterally. S1, S2 heard and no murmur.
Abdominal examination:
I need to expose patient from sternum level to midthigh, due to preserving patient's dignity and modesty, I will expose the patient from sternum till inguinal region.
Inspection
The abdomen was not distended and move along with respiration. There were no visible veins, no visible peristalsis and no surgical scar noted. Umbilicus was centrally located. Cough impulse was negative.
Palpation
A. Superficial: Abdomen was soft, tender and guarding at hypogastric and right inguinal region.
B. Deep:
1. Rovsing's sign +ve
2. McBurney's sign +ve
3. Rebound tenderness +ve
4. Psoas and Obturator Sign negative.
5. No hepatomegaly or splenomegaly.
6. Kidney ballottement was done and not ballotable
Percussion
Resonance in all regions.
Auscultation
Normal intensity of bowel sound
No renal or aortic bruit
Provisional diagnosis: Acute Appendicitis
During the discussion, examiners asked so many questions. My examiners were Mr. T and Dr. Ali. I'm blessed to have them as my examiners. They were so chill and cool.
Mr. T asked me most of the questions.
Discussions:
1. What are the differential diagnosis?
a. Acute Appendicitis
b. Mesenteric Adenitis
2. What do you want to look at the throat in relation with abdomen examination?
Injected throat in case of mesenteric adenitis because mesenteric adenitis always associated with upper respiratory tract infections.
3. What is Traube's space?
It's a crescent-shaped space overlying the stomach. The surface markings for Traube’s space :
- the left sixth rib,
- the left mid-axillary line and
- the left costal margin.
Percussion should be carried out at one or more levels of Traube’s space from medial to lateral.
Anatomical boundaries are:
1. Right: the inferior margin of the left lobe of the liver.
2. Left: the anterior border of the Spleen.
3. Superior: lower edge of the left lung (Resonance of lung).
4. Inferior: Costal margin.
2. Left: the anterior border of the Spleen.
3. Superior: lower edge of the left lung (Resonance of lung).
4. Inferior: Costal margin.
Contents
1. Fundus of the stomach (Hence percussion of Traube's area normally gives Tympanic note).
2. The costo-phrenic recess of left pleura devoid of lungs.
2. The costo-phrenic recess of left pleura devoid of lungs.
- Underneath lies the stomach, which produces a tympanic sound on percussion (medicine). If percussion over Traube's space produces a dull tone, this indicates splenomegaly
- This maneuver has a sensitivity and specificity between 60 and 70% for splenetic enlargement; however, the sensitivity and specificity increases to approximately 80% in non-obese patients who are fasting.
Other Causes of dull sound on percussion of Traube's space:
A. Full stomach.
B. Left sided Pleural effusion.
C. Enlargement of left lobe of liver due to any etiology.
D. Dextrocardia.
E. Proliferative growth in fundus of stomach.
B. Left sided Pleural effusion.
C. Enlargement of left lobe of liver due to any etiology.
D. Dextrocardia.
E. Proliferative growth in fundus of stomach.
4. What is Rovsing's sign?
It is a palpation of the left lower quadrant may elicit pain in the right lower quadrant. If this occurs, it is said to be a positive Rovsing sign. Rovsing's original description was an attempt to distend the caecum and appendix by pushing on the left colon in an anti-peristaltic direction.
5. Where is McBurney's point and what is McBurney's sign?
McBurney's point is the name given to the point over the right side of the abdomen that is one-third of the distance from the anterior superior iliac spine to the umbilicus. This point roughly corresponds to the most common location of the base of the appendix where it is attached to the cecum.
Deep tenderness at McBurney's point, known as McBurney's sign, is a sign of acute appendicitis. The clinical sign of referred pain in the epigastrium when pressure is applied is also known as Aaron's sign. Specific localization of tenderness to McBurney's point indicates that inflammation is no longer limited to the lumen of the bowel (which localizes pain poorly), and is irritating the lining of the peritoneum at the place where the peritoneum comes into contact with the appendix.
Tenderness at McBurney's point suggests the evolution of acute appendicitis to a later stage, and thus, the increased likelihood of rupture. Other abdominal processes can also sometimes cause tenderness at McBurney's point. Thus, this sign is highly useful but neither necessary nor sufficient to make a diagnosis of acute appendicitis. Also, the anatomical position of the appendix is highly variable (for example in retrocaecal appendix, an appendix behind the caecum), which also limits the use of this sign as many cases of appendicitis do not cause point tenderness at McBurney's point. For most open appendectomies (as opposed to laparoscopic appendectomies), the incision is made at McBurney's point.
6. What is rebound tenderness?
Blumberg's sign also referred to as rebound tenderness, is a clinical sign that is elicited during physical examination of a patient's abdomen by a doctor or other health care provider. It is indicative of peritonitis. It refers to pain upon removal of pressure rather than the application of pressure to the abdomen.
7. How do you know if the spleen is enlarged?
The normal adult spleen lies immediately under the diaphragm in the left upper quadrant of the abdomen. It ranges in length from 6 to 13 cm.
Palpation During the Spleen Exam
Technique
- Start in RLQ (so you don’t miss a giant spleen).
- Get your fingers set then ask the patient to take a deep breath. Don’t dip your fingers or do anything but wait.
- When the patient expires, take up a new position.
- Note the lowest point of spleen below the costal margin, texture of splenic contour, and tenderness
- If the spleen is not felt, repeat with pt lying on right side. Gravity may bring spleen within reach.
Percussion During the Spleen Exam
Technique
NOTE: Percussion may indicate but does NOT confirm splenomegaly.
With the patient in supine position, percuss inferior to lung resonance to map out gastric tympany (i.e. Traube’s Space).
- This area is variable; however, tympanic extending laterally makes splenomegaly less likely.
- Dullness may indicate splenomegaly, solid gastric content, or colon content.
Splenic Percussion Sign (Castell’s Sign): Percuss the most inferior interspace on the left anterior axillary line (Castell’s Point).
This is usually tympanic. Ask patient to breath deeply.
- Remains tympanic on inspiration: Splenic Percussion Sign negative: splenomegaly less likely.
- Shift from tympanic to dullness: Splenic Percussion Sign positive: splenomegaly more likely.
8. Why do the patient came with slowly walking and bending forward? What are the pathophysiology behind this action?
Due to inflammation in contact with the psoas muscle.
9. What is the different between radiation and shifting of pain?
Shifted pain - Pain from original site migrate to another site. The original site then no more feeling pain.
Radiated pain - Pain from original site migrate to another site. Now both side is in pain.
10. Why is the pain radiated to right iliac fossa from the epigastric area?
Pain that "shifts" from the original site of onset to another location in the abdomen is most often associated with acute appendicitis where periumbilical or epigastric pain (visceral) that is present early in the course of the disease is replaced with right lower quadrant (somatic) pain later in the illness when the parietal peritoneum becomes involved with the inflammatory process.
Pain produced by irritation of the parietal peritoneum by duodenal contents leaking from a perforated duodenal ulcer may begin in the epigastrum and may migrate to the lower quadrants of the abdomen or pelvis depending on the pathway that the leaking material takes through the abdominal cavity.
11. How do you diagnose appendicitis?
Through good history taking and physical examination
12. How do you diagnose UTI?
Tests and procedures used to diagnose urinary tract infections include:
- Analyzing a urine sample. Your doctor may ask for a urine sample for lab analysis to look for white blood cells, red blood cells or bacteria. To avoid potential contamination of the sample, you may be instructed to first wipe your genital area with an antiseptic pad and to collect the urine midstream.
- Growing urinary tract bacteria in a lab. Lab analysis of the urine is sometimes followed by a urine culture. This test tells your doctor what bacteria are causing your infection and which medications will be most effective.
- Creating images of your urinary tract. If you are having frequent infections that your doctor thinks may be caused by an abnormality in your urinary tract, you may have an ultrasound, a computerized tomography (CT) scan or magnetic resonance imaging (MRI). Your doctor may also use a contrast dye to highlight structures in your urinary tract.
- Using a scope to see inside your bladder. If you have recurrent UTIs, your doctor may perform a cystoscopy, using a long, thin tube with a lens (cystoscope) to see inside your urethra and bladder. The cystoscope is inserted in your urethra and passed through to your bladder.
Rub your hand to make it warm. If you touch patient with a cold hand, it will lead to muscle spasm.
14. How you manage the patient if he first come to you in the ED?
Assess hydrational status
Assess vital signs
Treat symptomatically
Ask patient to fasting in case patient need to go for operation
15. What treatment will you offer to this patient?
Open appendectomy or laparotomy
16. Type and site of appendicitis? Which one is the most common site?
Site of appendicitis:
The appendix sits at the junction of the small intestine and large intestine. It's a thin tube about four inches long. Normally, the appendix sits in the lower right abdomen.
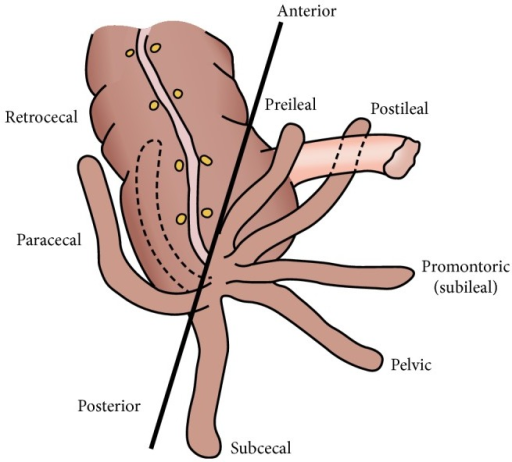
Type:
- Retrocecal (most common) 43.5%
- Subcecal 24.4%
- Post-ileal 14.3%
- Pelvic 9.3%
- Paracecal 5.8%
- Pre-ileal 2.4%
- Others 0.27%

















0 comments