- 5:07:00 PM
- 0 Comments

POST END POSTING EXAM - LONG CASE
Fuhhh, I just told you guys that I don't want stroke patient this morning right? Turn out I went to see my patient and suddenly my patient that I got is a stroke patient. WOW. What a case... I almost broke into tears and I became very nervous. Thank God, Liyana was there helping me out to prepare for the case. She did all the research while I try to memorise and smoothing my CNS physical examination flows.
Nina was there too and helping me out with the physical examination. I'm blessed to have friends like them. My subgroup-mates also very supportive and wish me luck with the patient.
I went to Mahsuri ward at 2.00 pm and starting to clerk the patient. Then I receive a message from Dr. Ong that I need to clerk Bed 15 instead Bed 2. I asked her for confirmation, and she said Bed 15 for me. Mann..
I called my friend and I told her our case had been swapped - giving her hints that she need to read about CNS examination and ischaemic stroke 2ry to cardioembolism instead CVS case.
He came due to left upper and lower limb muscle weakness.
My case - The CVS patient
The CNS CASE
The patient was a 65 year old malay gentleman but seems old from his age. He has underlying Chronic Rheumatoid Heart Disease, Chronic Kidney Disease and Gouty Arthritis.He came due to left upper and lower limb muscle weakness.
My case - The CVS patient
My patient was well cooperate and very friendly. 1 hour was not enough for me to clerk and did my examination (suprisingly!). 1 hour given to me was always enough before this, I wonder if changing my style by first listening to all the patient had to say is better than while listening I should jotted down everything and arrange it all together. Hmm. The latter seems better for me.
My patient was a 43 year old, malay gentleman working as hawker and live in Melor, Kota Bharu. He is a smoker with history of 21 pack years for more than 30 years. He stopped smoking last month.
Patient is a known case of hypertension and also hypercholesterolnemia. He was diagnose with hypertension since 2 years ago and not compliance to medication. His hypercholesterolnemia was diagnosed last month and claimed compliance to medication.
His main complaint was chest discomfort, breathlessness and lethargy. Then nothing. Aiyoo. There was 5 days history admission to CCU recently (last month) due to almost similar presentation but worsen than the current one. He was not aware of the diagnosis. But listening to his description about the symptoms is more likely like acute myocardial infarction or acute heart failure.
Upon physical examination, Apex beat was not displace (5th intercostal space, mid-clavicular line), there was thrills present at left sternal edge. Pansystolic murmur was heard best heard by diaphragm at mitral area and radiated to axilla - bloody hell it was mitral regurgitation! And I was so pleased with myself that I can finally differentiate the type of murmur. Bibasal crepitation was heard and there was no sacral and pedal edema.
My differential diagnosis were Acute Coronory Syndrome and also Heart Failure. Dr. Ong asked me about the investigation I would done and management for Acute Coronary Syndrome Disease. She gave me good mark, Alhamdullilah !
Investigation I would carry out :
1) FBC - looking for any infections from total white count and looking for anemia from Hb level.
2) Coagulation Test
3) Renal profiles
4) Liver Function Test
5) Cardiac Biomarkers - Troponin & CKMB
6) ECG - ST elevation in Myocardial Infarction
7) Chest X-Ray - to look for any cardiomegaly or other underlying disease
8) Echocardiogram - To see the LVEF status, cardiac wall, cardiac contractility and to confirm mitral regurgitation
Management:
1) Airway
2) Breathing
3) Circulation
4) Give oxygen if patient still breathlessness
5) Primary PCI
6) Anti-fibrinolytic such as streptokinase or ateplase
7) Anti hypertensive drug - Frusemide
8) Educate patient
💕 READ HOW TO DIFFERENTIATE MURMURS 💕
HERE
- 6:55:00 PM
- 0 Comments

Cushing’s Triad is a clinical triad described with bradycardia, Systolic hypertension and irregular breathing. It is named after Harvey William’s Cushing, who actually demonstrated Cushing's reflex (again him) first.
Cushing’s Reflex is the physiological phenomena, in which raised intracranial pressure leads to irregular breathing, bradycardia and systolic hypertension/ increased wide pulse pressure. Cushing’s Reflex is also known as Cushing’s Effect, Cushing’s Reaction, Cushing’s Phenomenon and Cushing’s Law.
MECHANISM
The Cushing reflex is complex and seemingly paradoxical. The reflex begins when some event causes increased intracranial pressure (ICP). Since the cerebrospinal fluid is located in an area surrounded by the skull, increased ICP consequently increases the pressure in the fluid itself. The pressure in the cerebral spinal fluid eventually rises to the point that it meets and gradually exceeds the mean arterial blood pressure (MABP or MAP). When the ICP exceeds the MABP, arterioles located in the brain's cerebrum become compressed. Compression then results in diminished blood supply to the brain, a condition known as cerebral ischemia.
During the increase in ICP, both the sympathetic nervous system and the parasympathetic nervous system are activated. In the first stage of the reflex, sympathetic nervous system stimulation is much greater than parasympathetic stimulation. The sympathetic response activates alpha-1 adrenergic receptors, causing constriction of the body's arteries. This constriction raises the total resistance of blood flow, elevating blood pressure to high levels, which is known as hypertension. The body's induced hypertension is an attempt to restore blood flow to the ischemic brain. Sympathetic stimulation also increases the rate of heart contractions and cardiac output. Increased heart rate is also known as tachycardia. This combined with hypertension is the first stage of the Cushing reflex.
Meanwhile, baroreceptors in the aortic arch detect the increase in blood pressure and trigger a parasympathetic response via the vagus nerve. This induces bradycardia, or slowed heart rate, and signifies the second stage of the reflex.[Bradycardia may also be caused by increased ICP due to direct mechanical distortion of the vagus nerve and subsequent parasympathetic response. Furthermore, this reflexive increase in parasympathetic activity is thought to contribute to the formation of Cushing ulcers in the stomach, due to uncontrolled activation of the parietal cells. The blood pressure can be expected to remain higher than the pressure of the raised cerebral spinal fluid to continue to allow blood to flow to the brain. The pressure rises to the point where it overcomes the resisting pressure of the compressed artery, and blood is allowed through, providing oxygen to the hypoxic area of the brain. If the increase in blood pressure is not sufficient to compensate for the compression on the artery, infarction occurs.
Raised ICP, tachycardia, or some other endogenous stimulus can result in distortion and/or increased pressure on the brainstem. Since the brainstem controls involuntary breathing, changes in its homeostasis often result in irregular respiratory pattern and/or apnea. This is the third and final stage of the reflex.
Commonly, in various pressor reflexes, the central chemoreceptors, which transform chemical signals into action potentials, and the baroreceptors, which sense pressure changes of the carotid sinuses, work together to increase or decrease blood pressure. However, chemoreceptors do not play a role in the Cushing reflex. Thus, even in the presence of sympathetic stimulation from the brain, which would normally produce tachycardia, there is in fact bradycardia.

FUNCTION
Raised intracranial pressure can ultimately result in the shifting or crushing of brain tissue, which is detrimental to the physiological well being of patients. As a result, the Cushing reflex is a last-ditch effort by the body to maintain homeostasis in the brain. It is widely accepted that the Cushing reflex acts as a baroreflex, or homeostatic mechanism for the maintenance of blood pressure, in the cranial region.
Specifically, the reflex mechanism can maintain normal cerebral blood flow and pressure under stressful situations such as ischemia or subarachnoid haemorrhages. A case report of a patient who underwent a spontaneous subarachnoid haemorrhage demonstrated that the Cushing reflex played a part in maintaining cerebral perfusion pressure (CPP) and cerebral blood flow. Eventually, the ICP drops to a level range where a state of induced hypertension in the form of the Cushing reflex is no longer required. The Cushing reflex was then aborted, and CPP was maintained. It has also been shown that an increase in mean arterial pressure due to hypertension, characteristic of the reflex, can cause the normalization of CPP. This effect is protective, especially during increased intracranial pressure, which creates a drop in CPP.
REFERENCE:
- 11:52:00 PM
- 0 Comments

Hi guys, I'm a 4th year medical student from Lincoln University College. Currently in Internal Medicine posting for 4 weeks. This is my second week in this posting and gotta share what I learnt last week.
Four groups has been assigned to four different Medicine wards in Hospital Raja Perempuan Zainab (HRPZ) II; Mahsuri, Bendahara, ward 8/8P and also Puteri. My first week is at Ward Mahsuri.
Then, Dr. Azza gave us a list of specialist in charged for each group. My group was assigned to few specialist there, including Dr. Sinari. She is the consultant of Medicine department. Our favourite specialist for time being is Dr. Grace from Mahsuri ward. She is so nice, graceful and very knowledgeable. She treat her medical officer and houseman so nice that I felt lucky to have her as one of our group specialist in-charged. Bless us. Bless me.
First day was tiring but there was no bed side teaching. Second day of first week, we went to the ward and introduce ourself to the staffs there. Most of the houseman there are very nice. They include us in every ward round and help us whenever we look blur in the cubicle. The medical officer in charged for cubicle 3 in ward Mahsuri is Dr. Mohd. He is the coolest person there. I mean, as a medical officer, he really concern about the patient and also the houseman under him. Those houseman under him and Dr. Grace were lucky. Other medical officer in the ward that I find very amusing is Dr. Hidayah. She is so rock and cool. She got this mighty confident and a very unique lady, I must say.
During ward round, Dr. Grace will include us in the discussion as well. She ask questions and also explain about the case, the decision-making, and also the insight of that case. Dr. Mohd also help us and discuss the case briefly so that we understand the case well when the ward round take place. For the first time, I felt like being welcomed by the specialist, medical officer and also all the staffs there. They are too nice. I can't believe that I'm in medicine posting.

We were given homework at the end of ward round. For me, it is more like a reading list or list of topics that you need to read at home. So here are the list for the 1st week of posting:
1. Hypertensive Intracranial Bleeding 👌
2. Atypical Pneumonia 👌
3. Community Acquired Pneumonia 👌
4. Retroviral Disease 👌
5. Upper GI Bleed
6. Status Epilepticus
👌 = DONE
Till now, I haven't touch those last two topics. Hahaha. Sigh. Then we went for a clinic session. First clinic session was a rheumatology clinic. But we were some sort of not welcomed and kena marah in front of the patient inside the doctor's room. I almost cry but kinda tahan because the fault was not from our side. We did all the things that we need to do; we introduce ourself at the counter. We ask who in-charged for the clinic. We introduce ourself again to the nurses in the doctor's clinic and asked for permission. The person in-charged was not there so we waited outside. Suddenly the nurse came to us and informed us that we can asked for permission from the doctors in the other room. So we all went inside the room and again, introduce ourself to the two medical officers inside that tiny room. It was so crowded. One of the doctor told us to clerk a patient who is currently waiting outside the room. So yeaa. We clerked. We followed the patient went inside meeting other medical officer. And then after everything almost end, a lady came inside the room and marah us for not introducing ourself. We were so puzzled that time as we already did the introduction part and still kena marah. We explained and she was like still perli us about not respecting the clinics. They were not informed yada yada. Sigh. Sometime you buat everything also kena marah. So yeaaa whatever.
Another clinic experience is with Dr. Pong from Respiratory Clinic. She was so nice, so cute, so cool and so friendly with the patient, including us. We sit inside the room and she will ask questions related to each patient that came to see her. We felt like we were welcomed and she teaches us about pulmonary fibrosis that day.


Here are my second week posting reading list:
1. Cushing reflex 👌
2. Renal with hepato involvement
3. Typhoid Fever
4. Pott's Disease
5. Liver Cirrhosis
6. Obstructive Jaundice
7. Upper GI Bleed
8. Status Epilepticus
Date: 18 March 2018
1. Hypergylcemic Hyperosmolar State (HHS) 👌
2. Hypoventilation Obesity Syndrome
3. Cardiomyopathy 👌
4. Uremia
5. Delirium vs Dementia
6. Congestive Heart Failure 👌
7. Upper GI Bleed
8. CVS Murmur Maneuvers 👌
Date: 19 March 2018
1. Asthma / COPD
2. Respiratory Failure
3. CNS Examination
4. Causes of stroke
👌 = DONE
So many things to cover right ?
- 10:56:00 PM
- 0 Comments

- 6:57:00 PM
- 0 Comments


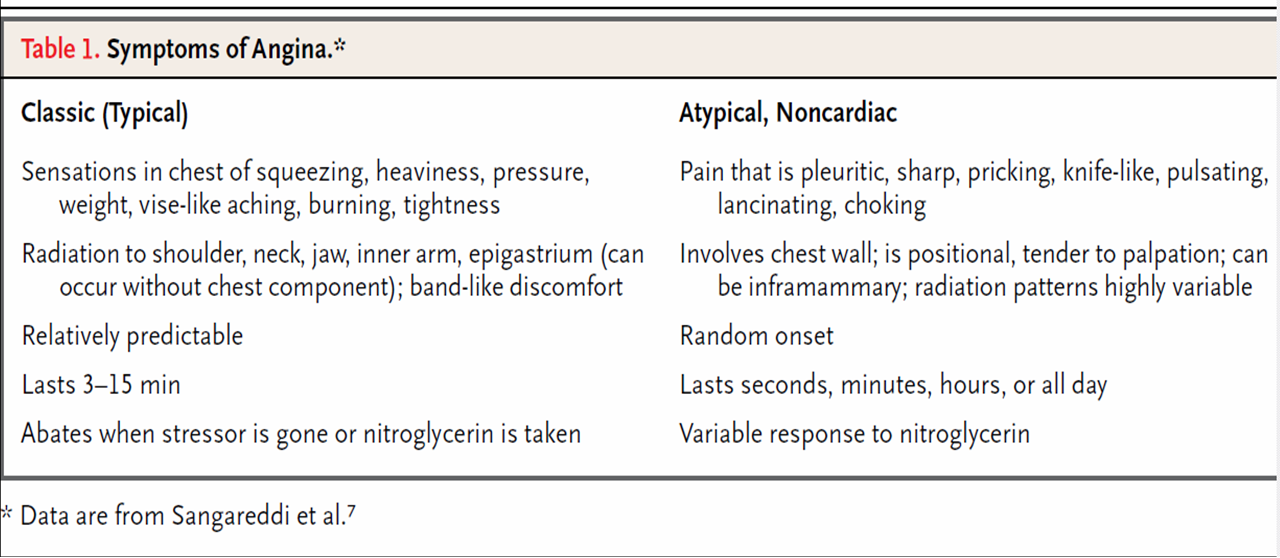
Distinguishing between Cardiac and Non-Cardiac Chest Pain
There is no conclusive way to differentiate between cardiac and non-cardiac chest pain in the home environment. There are many cases where severe heartburn causes chest pain that resembles cardiac disease and only the use of nitrates may allow a person to differentiate between cardiac and non-cardiac chest pain in this instance. Severe chest pain should always be taken seriously and a trip to the emergency room is often warranted to exclude more serious underlying disorders. This can only be done under the supervision of a medical professional in conjunction with the relevant tests and investigations. Refer to Chest Pain Tests and Chest Pain Diagnosis for more information.
Nature
- Cardiac
- Pain is dull, constricting, choking and/or crushing.
- Other terms to describe ischemic cardiac chest pain includes squeezing, burning or heavy.
- Sometimes it may just feel like discomfort which is why the character of cardiac chest pain can be so misleading.
- A common but inconclusive presentation in cardiac chest pain is a patient clutching the chest
- Non-Cardiac
- The pain may vary from burning to sharp, stabbing and prickling.
- Chest pain due to anxiety may also result in pain that is similar to cardiac chest pain.
Location
- Cardiac
- The pain is usually central (towards the center of the chest) and fanning outwards (diffuse).
- Non-Cardiac
- Pain may be away from the center of the chest where a patient can clearly identify it as a right-sided or left-sided chest pain.
- Pain is usually localized – located at only one spot which can be clearly pinpointed by the patient.
Radiation
- Cardiac
- Pain to the jaw, neck, shoulder, arms (either one or even both) or back.
- Sometimes there pain may be radiated to the upper abdomen.
- Non-Cardiac
- There may not often be any radiation of the pain or it may radiate to other sites apart from those mentioned above.
- Gastritis with accompanying GERD may cause a burning chest pain as well as upper abdominal pain and this may be confused for radiation.
Precipitating Factors
- Cardiac
- Triggered or exacerbated by exertion or emotion.
- At times a large meal or even extremes of temperature, particularly cold, can trigger or exacerbate the pain.
- Unstable angina may not be triggered by any specific factors.
- Non-Cardiac
- Spontaneous although it may be exacerbated by exertion (usually after rather than during activity).
- Changes in posture, deep or rapid breathing or pressure may also exacerbate the pain.
Relieving Factors
- Cardiac
- Pain is relieved by rest and responds quickly to nitrates.
- Non-Cardiac
- Not relieved significantly by rest, if at all.
- Does not respond to nitrates or there may be a slow response.
- Pain relived by antacids may be related to gastrointestinal disorders. Pain that improves upon leaning forward may be related to the pericarditis (inflammation of the lining around the heart).
Concomitant/Associated Signs and Symptoms
- Cardiac
- Severe shortness of breath – patient may report a feeling of suffocation.
- Dizziness
- Fainting spells (‘blackouts’)
- Non-Cardiac
- Other signs and symptom may be present that is helpful in identifying the cause of the pain.
- Gastrointestinal – bloating, belching, nausea, vomiting and/or regurgitation. Refer to Gastric Chest Pain.
- Respiratory – shallow breathing, persistent cough, abnormal breathing sounds, difficulty breathing when lying flat, expectorating mucus or coughing up blood. Refer to Lung Chest Pain.
- Musculoskeletal – limited range of motion, cannot tolerate pressure on the affected area. Refer to Muscle Chest Pain and Bone Chest Pain.
- Psychological – weepy, depressed, excited, agitated, fearful. Refer to Nerve Chest Pain.





- 2:14:00 AM
- 0 Comments

Congenital Cardiovascular Defects
Statistical Fact Sheet 2016 Update (American Heart Association)
Congenital cardiovascular defects, also known as congenital heart defects, are structural problems
that arise from abnormal formation of the heart or major blood vessels. ICD-9 lists 25 congenital heart
defects codes, of which 21 designate specified anatomic or hemodynamic lesions. Defects range in
severity from tiny pinholes between chambers that may resolve spontaneously to major malformations
that can require multiple surgical procedures before school age and may result in death in utero, in
infancy, or in childhood.
The common complex defects include the following:
- Tetralogy of Fallot (TOF)
- Transposition of the great arteries
- Atrioventricular septal defects (ASD)
- Coarctation of the aorta
- Hypoplastic left heart syndrome
Incidence
- Congenital heart defects are serious and common conditions that have significant impact on morbidity, mortality, and healthcare costs in children and adults.
- The most commonly reported incidence of congenital heart defects in the United States is between 4 and 10 per 1,000, clustering around 8 per 1,000 live births.
- Continental variations in birth prevalence have been reported, from 6.9 per 1000 births in Europe to 9.3 per 1000 in Asia.
- An estimated minimum of 40,000 infants are expected to be affected each year in the United States. Of these, about 25%, or 2.4 per 1,000 live births, require invasive treatment in the first year of life.
Mortality
Mortality related to congenital cardiovascular defects in 2013 was 3,051. Any-mention mortality
related to congenital cardiovascular defects in 2013 was 4,916.
Risk Factors
Numerous intrinsic and extrinsic non-genetic risk factors contribute to congenital heart defects.
- Known maternal risks include maternal smoking during the first trimester of pregnancy. Exposure to secondhand smoke has also been implicated as a risk factor.
- Maternal binge drinking is also associated with an increased risk of congenital cardiac defects, and the combination of binge drinking and smoking may be particularly dangerous.
- A greater risk of congenital heart defects is also seen in women who both have a high BMI. Gestational DM has also been associated with cardiac defects, both isolated and multiple.
- Folate deficiency is a well-accepted risk for congenital defects, including congenital heart defects, and folic acid supplementation is recommended during pregnancy






- 1:52:00 AM
- 0 Comments



- 7:29:00 PM
- 0 Comments



So today is all about the heart. What about it? I'm gonna share to you gaisssss few videos that had been helping me a lot while I'm studying. Of course it is from the youtube channels. The easiest video channel you can search to. Let's start from scratch.
First, you need to know and understand the anatomy of heart. The landmark and the area of heart. If you go to a new place, you need to know the area, the places and the landmarks right in order to know that new place. So that you won't get lost.
First, you need to know and understand the anatomy of heart. The landmark and the area of heart. If you go to a new place, you need to know the area, the places and the landmarks right in order to know that new place. So that you won't get lost.

Then we proceed to the physiology of heart. This time, you need to know and understand (and memorize as well!) about the function of heart and how it works normally. If you don't know the normal function of heart, how will you distinguish it with the abnormal function?
Do you know how to interpret electrical activity of the heart? We use ECG to monitor the electrical activity of the heart. So what is ECG?
For me, I really like the '11 steps to read an ECG'. It's the same as Dr. Nik taught us in the class. The systems or the steps that needed to read an ECG.
11 steps:
- Rhythm
- Rate
- Axis
- P-wave
- P-R Interval
- QRS complex
- Q wave
- R wave
- S wave
- S-T segment changes
- T wave








Wanna try to label all those organs? :D

- 7:20:00 PM
- 0 Comments

Prof Mazlin is here. I think she is so cool, she made everything so simple. Just now she taught us about history taking and physical examination according to her way. Last time we learnt from Prof. Nazmi according to his way. Their ways are more or less the same. I'd prefer Prof. Mazlin's way.

- 5:40:00 PM
- 0 Comments
M Y . I N T E R N A L . M E D I C I N E . S C H E D U L E

Sobs sobs, so pack ! This is for the first 4 weeks out of 8 weeks of Internal Medicine Posting in Tanah Merah. First four weeks are the toughest week as it include the respiratory system, cardiovascular system, GIT system, haematology and cranial nervous system.
The other remaining four weeks will be the endocrine system, renal system and miscellaneous. Mannnn, I need to study from the beginning as this posting required a lot of reading, memorize facts and understanding skills. *cry*
End posting exam is a week after raya puasa. How can I enjoy this year Hari Raya Aidilfitri? Still wondering which week should I sacrifice.. hehehehe..
End posting exam is a week after raya puasa. How can I enjoy this year Hari Raya Aidilfitri? Still wondering which week should I sacrifice.. hehehehe..
- 4:05:00 PM
- 0 Comments


- 6:44:00 PM
- 0 Comments

















